Increasing and sustaining vaccination uptake is vital for vaccines to achieve their success. Achieving high vaccination coverage requires an understanding of the drivers of immunization uptake, engaging with communities to apply tailored evidence-based strategies to improve uptake and strengthen the quality of services. To determine the impact and sustainability of the interventions monitoring and evaluation is also necessary.
This page provides a range of evidence-based guidance for programmes and partners to guide the implementation and evaluation of strategies to increase vaccine demand and uptake. The content and guidance on this page is curated and maintained by the Demand and Behavioural Sciences team, within the Essential Immunization Programme, WHO Department of Immunization, Vaccines and Biologicals.
- Understand the drivers of immunization uptake
- Engage with communities
- Strengthen the quality of services
- Support health workers
1. Understand the drivers of immunization uptake
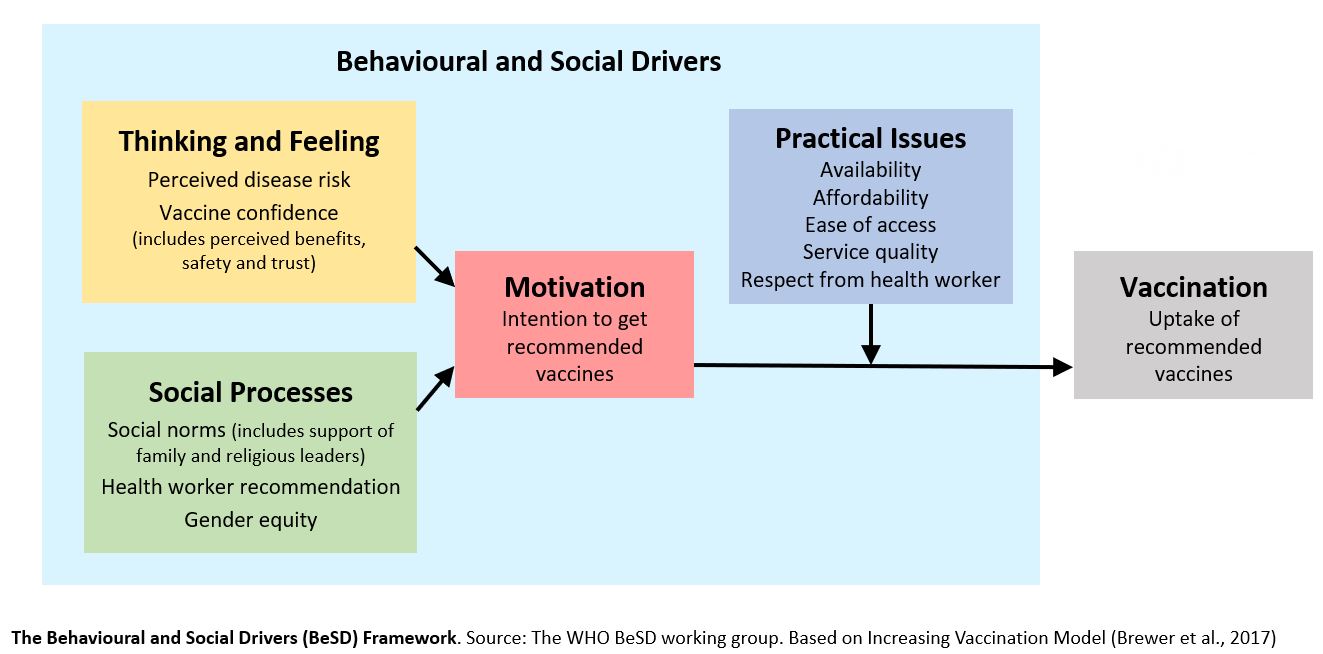
A range of factors influence whether a person is vaccinated or not. The framework of behavioural and social drivers (BeSD) of vaccination (see below chart) illustrates the four domains that can be measured to understand reasons for under-vaccination. The BeSD framework includes influences that are measurable, potentially changeable, and specific to vaccination.
Behavioural and social drivers of vaccine uptake: tools and practical guidance
Understanding the behavioural and social drivers of vaccine uptake. WHO position paper – May 2022
For added BeSD tools, guidance, and case examples, click here.
Figure 1. Behavioural and social drivers of vaccination framework
2. Engage with communities
Because the drivers of uptake are contextual, assessing and addressing low uptake requires engaging with communities to generate insights on their needs and perspectives, and to guide the development of better quality vaccination services, systems, policies, and other programme strategies.
Human Centred Design for Tailoring Immunization Programmes (HCD-TIP) is an approach for working with communities to close coverage gaps and overcome inequities for vaccination in four stages: Diagnose, Design, Implement and Evaluate.
HCD-TIP can be used for any priority group or vaccine across the life course and enhances the ability of programmes to listen and learn to better respond to community needs.
Human-centred design for tailoring immunization programmes: a practical guide
3. Strengthen the quality of services
Very often it is practical issues, and not a lack of confidence or motivation, that is the cause of low uptake. Practical issues include the experiences that people have in trying to get vaccinated, including barriers faced, e.g., accessing the health facility, or costs of transport.
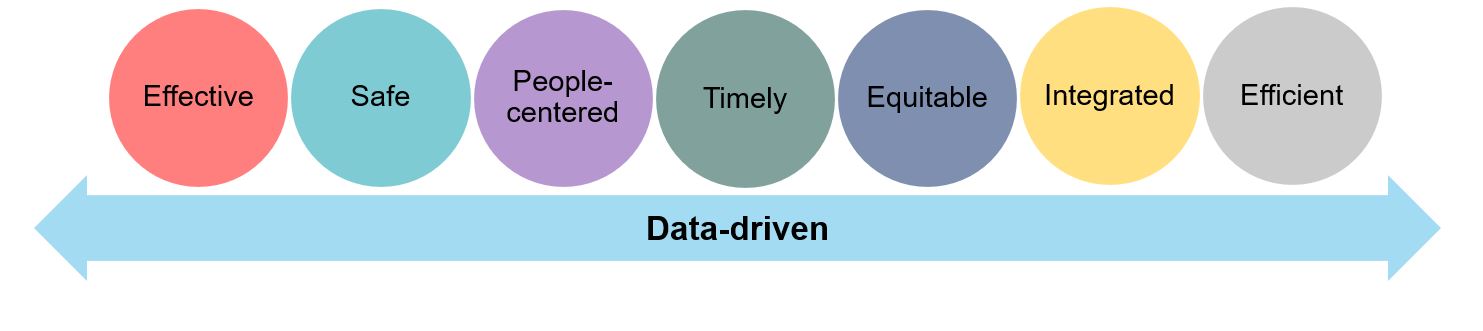
The Quality Immunization Services Planning Guide highlights key actions at different levels of the health system to monitor, strengthen, and maintain the quality and convenience of services.
Benefits of strengthening immunization service quality include enhanced health service and system performance, improved vaccination coverage and efficiency, and more equitable access to services to reduce gaps for disadvantaged populations.
Quality immunization services: a planning guide
Figure 2: Guiding principles of quality immunization services
4. Support health workers
As the most trusted influencer of vaccination decisions, it is important health workers are well prepared and supported in the demands of their role. The capacity and confidence of health workers are often stretched as they are faced with time constraints, limited resources, and inadequate information and/or training to respond to questions and discuss the benefits and rare risks of vaccination.
To build capacity in managing pain during vaccination and in engaging in difficult conversations with hesitant caregivers, two specific and adaptable trainings are available:
Health worker training module: managing pain during vaccine administration (pptx, 3Mb)
Health worker training module: conversations with hesitant caregivers (pptx, 910kb)